Bruxism, TMD, Jaw Clenching and Teeth Grinding
Bruxism and Temporomandibular Disorder, or TMD, a condition which affects the temporomandibular joint (TMJ) all came to the forefront of dentistry during the 2020 coronavirus pandemic. This is because people and many of our dental patients felt increased stress due to health worries, financial worries, and the close proximity of family members during lockdown.
Anyone suffering extreme stress is likely to experience jaw clenching and teeth grinding which can happen at night during sleep without the sufferer being aware of the oral exercise. This activity can rapidly wear down teeth, but there are certain dentist-approved remedies to help mitigate the damage and self-help measures like stress reduction and mindfulness which can effectively cure the problem. Either way, the path to wellness begins with your dentist.
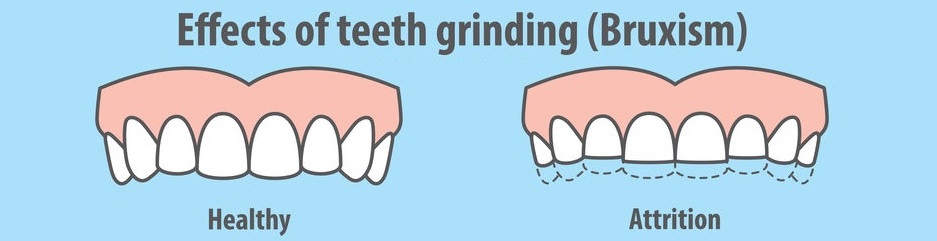
Stress and anxiety are unhealthy, and dentists are first to observe the damage it causes the human body. Not only does the friction rapidly deteriorate teeth, it’s often associated with other more serious illnesses. Oral health professionals at Archer Dental can spot patients who are suffering bruxism (teeth grinding) and temporomandibular disorders (TMD) by the worn condition of their teeth.
How do temporomandibular disorders (TMD) affect sufferers?
The most common signs of TMD are soreness around the patient’s ear, jaw joint, and jaw-muscles. Other symptoms relate to soreness and noises when opening or closing the mouth. Jaw bones make clicking or crunching noises when the patient chews, or yawns or opens their mouth for any reason.
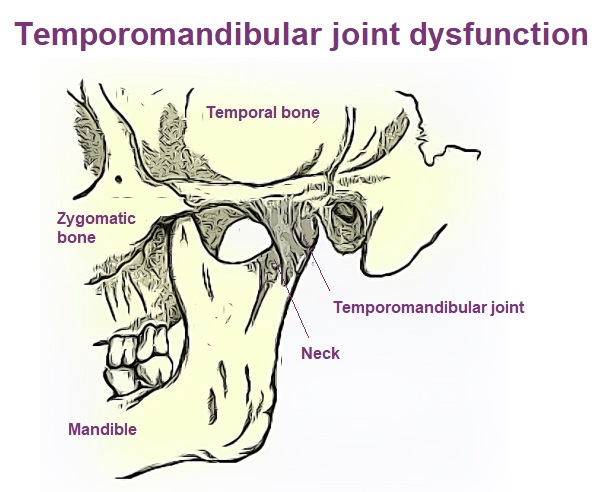
TMDs may be linked with neck pains and headaches and sometimes people feel discomfort in their temples or in their teeth. If you have any of these symptoms, report your condition to your dentist or physiotherapist.
Dental maladies such as teeth grinding, jaw clenching, and jaw pain were more common during the COVID-19 pandemic because people were really stressed.
The temporomandibular joint (TMJ) is the name of the joint located on either side of your head, just in front of your ears. These joints connect your mandible (jawbone) to your temporal bone (skull).
The temporomandibular joint can rotate backwards, forwards, and from side to side; it’s considered one of the most complex joints in the human body. This flesh to bone intersection, a tangle of muscles and ligaments, facilitates chewing, speaking and swallowing. When we have a problem with either the muscle, or bone or other tissue in the area of the TMJ, it’s considered a temporomandibular disorder or TMD.
How does Archer Dental treat TMD?
If you struggle with headaches, jaw or face pain, or the effects of jaw-clenching and teeth grinding, and you believe you may have a TMD, then professionals at Archer Dental can provide treatment options. Oral health care providers will examine your teeth and jaw and perform tests including x-rays to determine the exact nature of your ailment. If we diagnose a TMD, then we can help with treatment plans that may include:
Night guards reduce damage to teeth because they prevent TMD sufferers from grinding their teeth while they sleep and further aggravating their sore jaws at night.

A plastic night guard is a custom fit device which prevents those afflicted with TMD’s from doing further damage to their dental work, but it doesn’t cure the problem.

A sport mouth appliance can be made for patients who grit their teeth while playing sports or doing physical work.
Pain medications can help ease the symptoms and give temporary relief.
Dentists can also refer patients to specialists like certified physiotherapists or chiropractors to help ease muscle pain and correct misalignment.
A behavioral therapist may be recommended to help find ways to deal with stress and help calm the tension that is causing the TMDs.
BOTOX® for Bruxism at Archer Dental
BOTOX® is used as an alternative treatment for TMD and associated jaw tension and pain. Botox, otherwise known as Botulinum toxin type A, is a form of Clostridium botulinum (a bacterium) that has been purified for medical use. When this material is injected into TMJ region muscles it can help them relax, which relieves headaches, migraines, and jaw joint issues that stem from TMD, bruxism, and stress related clenching or teeth grinding.
Botox usually takes effect between one to three days after injection, but in some cases it can take up to two weeks to feel the benefits. The positive effects can last between three to six months.
Archer Dental has certified BOTOX Injection Professionals

Dentists have real-world experience dispensing therapeutic BOTOX® injections to the face and neck. Only such an experienced BOTOX Injector who has completed continuing education programs relating to the therapeutic and esthetic use of Botox can become certified. Our clinicians are well versed in the therapeutic effects and know best how to leverage esthetic benefits.
Botox works on a neuromuscular level to relax the muscles predisposed to clenching and grinding and reduces the contraction of those muscles so patients feel less pain in the area.
Botox also relieves painful headaches or migraines that are often caused by bruxism, and it can protect your teeth from fractures and the wear and reduction from grinding.
In our experience, TMDs will usually resolve themselves over time as life conditions change. But while suffering, our dental professionals can help stop the damage being done and bring some relief to sufferers.
Dentist supervised self-care for TMD
Treatments for TMD can include self-help. Archer Dental recommends patients do exercises at home and they offer these practical suggestions.
- Create either cold or warm compresses (whichever feels better) to help ease sore jaw muscles. Carefully apply the compress to the affected area to ease the pain and gain movement in your jaw area.
- Try to minimize the movement of your jaw and this may require only eating soft foods for some time. Explore protein shakes or nutrient rich meal replacements; this is a temporary approach for acute pain.
- Avoid yelling or singing carols while your TMJ region is healing.
- Stop chewing gum, nuts or beef jerky, as these actions require repetitive motions that may aggravate the muscles in the region.
- When sleeping, avoid putting pressure on your jaw, remember to lie with head up instead of resting chin on hand, pillow, or partner.
- Learn to use your tongue to keep your teeth slightly apart; this will minimize clenching and grinding, especially during exercise.
- Breathe properly and take warm baths, walks, and try to remain calm.
Physiotherapists can remedy orofacial pain

Many sufferers use physiotherapy to eliminate TMJ pain. A trained physiotherapist can perform more detailed assessments of a patient’s TMJ problem and more accurately match the treatment plan to the root cause.
Some patients have a TMJ joint that moves too easily, and too much or in a poor pattern. Experienced physiotherapist can recognize this problem and design treatments with exercises that strengthen weak muscles and improve mouth and jaw movement patterns.
POSTURAL TRAINING or simply changing a patient’s forward head posture can help some people who suffer from TMJ dysfunction. Physiotherapists teach patients how to strengthen postural muscles and lengthen shortened tissues so that they can improve their head position.
PAIN RELIEF for TMJ DYSFUNCTION? When patients are in a lot of pain and just need some relief so that they can begin to make the changes outlined above, a physiotherapist can help relieve the pain with thermal modalities, acupuncture and gentle manual therapy.

